The comparison of index cancer burden data in China and the United States, screening is an important factor!
Author:Cancer Channel of the Medical Time:2022.08.01
*For medical professionals for reading reference

Teach you how to scientifically screen!
Colorectal cancer (CRC) is the third largest and most common cancer in the world, and it is also the second major cause of cancer death. In 2020, there are about 1.93 million new colorectal cancers and 940,000 deaths. [1] CRC's burden is closely related to socio -economic status [2]. In recent years, changes in economic development and lifestyle and dietary habits have increased the incidence and mortality of China's CRC.
The "medical circles of tumor channel" compared the differences in the survival data of colorectal cancer in China, the United States and Europe, and analyzed the role of screening in CRC patients: screening to detect CRC patients is better than non -screening detection CRC. ?
The trend is very different, and China's actions are urgent.
Globocan 2020 estimates that the incidence of CRC ranks third in China and Europe, ranking fourth in North America [1].
The age of age (ASI) (ASI) (23.9/100,000) is higher than the world average incidence (195/100,000), while ASIR in Europe and North America is higher (304/100,000 and 262/100,000).
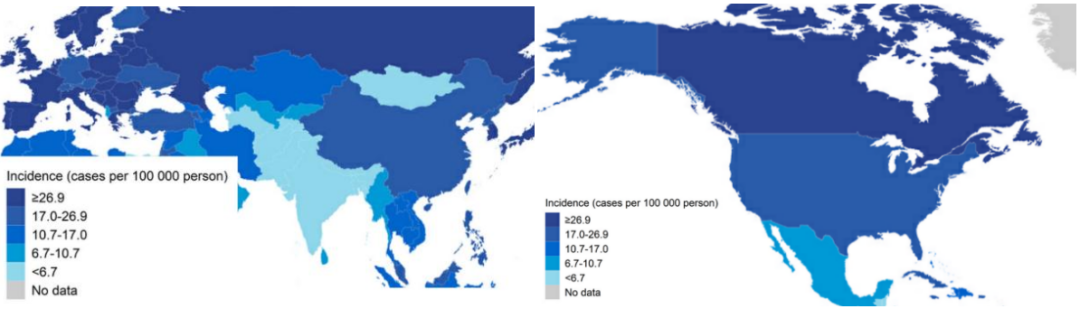
Fig
China's CRC age standardization (ASMR) (12.0/100,000) and Europe (12.3/100,000) are higher than the world average (9.0/100,000). ASMR in North America (8.2/100,000) is slightly lower than the world average.

Fig
Figure 3, Figure 4 [3] lists the detailed trend of the incidence and mortality rate of the CRC in the past 20 years. Considering the trend mode of the incidence and mortality, the countries incorporated into three categories are divided into three categories.
CRC's incidence rising or stable but declining mortality: Canada and most European countries are currently undergoing.
The incidence and mortality of CRC have declined: the United States and Austria, Czech Republic, Germany and other European countries.
The incidence and mortality rate of CRC are increased: In China, the average incidence of men and women has a average annual percentage percentage of the incidence of 1.6 and 0.0, respectively, and the AAPC of men and women's mortality is 1.3 and 0.6, respectively.

Figure 3 The incidence and mortality rate of CRC in the middle, Europe, and the United States CRC in the middle and twenty years, China is growing up
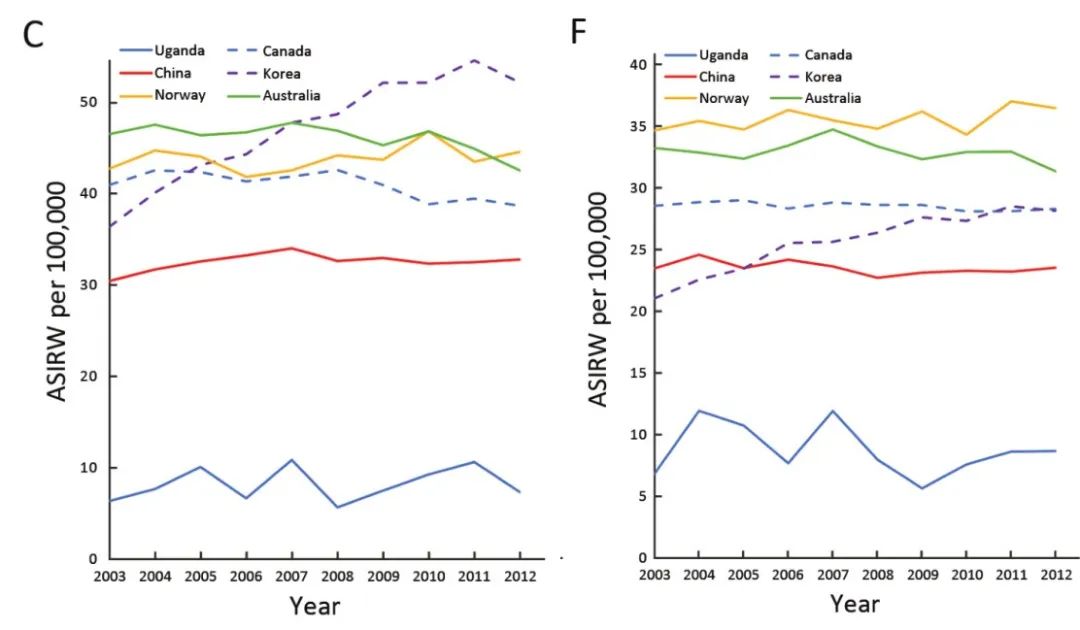
Figure 4C.2003-2012 The incidence of men's colorectal cancer in men's sexual colorectal cancer Figure 4F.2003-2012 The incidence of female sex colorectal cancer in the middle of the middle of the country, the world standard population age standardization incidence
Thanks to the development and progress of medical technology, the five -year survival rate in the three regions has increased.
In China, the age standardization rate of CRC patients in 2012-2015 has a relatively 56.9%relative survival rate of 56.9%, which has continued to rise since 2003. [4]
In Europe, the average age standardization of colon cancer and rectal cancer from 2000 to 2007 was 57.0%and 55.8%[5].
In the United States, the 5-year relative survival rate of CRC increased from 50%in the mid-1970s to 64%from 2009-2015 [6].
Generally speaking, compared with developed countries in Europe and the United States, the prevalence, mortality, and 5 -year survival rate of CRC in my country must be a little worse, and the prevalence and mortality rates have risen. Improved.
High prevalence is related to my country's large population, rapid economic development, and aging population. The developed countries have gone through this process to explore some screening plans to screen the incidence of CRC in Europe and the United States. What about the trend?
Is it good to screen? The data is here!
A large -scale study results obtained from 16 European countries in the 16 European countries of the 9 European countries showed that the screening and detection of CRC patients and non -screening detection of CRC's survival data were displayed. The results showed that patients with CRC were better prognosis [7].
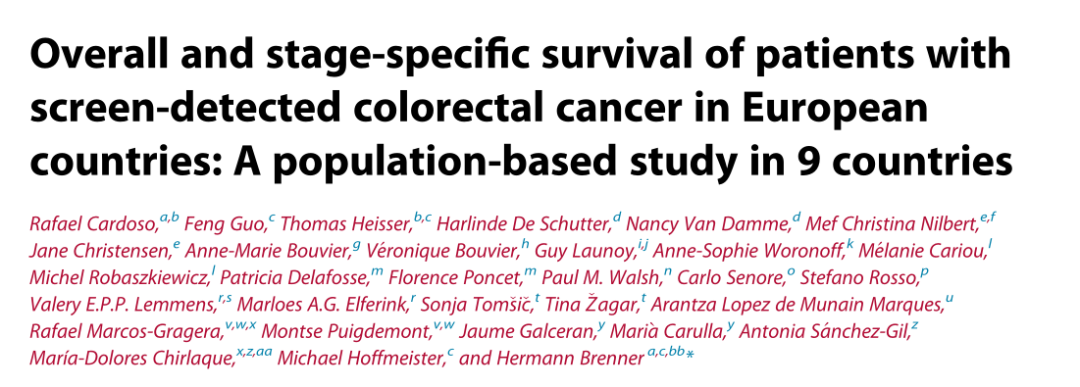
Figure 5 Thesis Homepage Screenshot
Compared with the detected CRC patients, the detection of CRC patients in patients with CRC patients is higher (43.0%vs18.6%); the detection rate of stage IV is low (7.6%vs18. 6%) (Figure 6); the prognosis of each staging of cancer is also better (Figure 7).
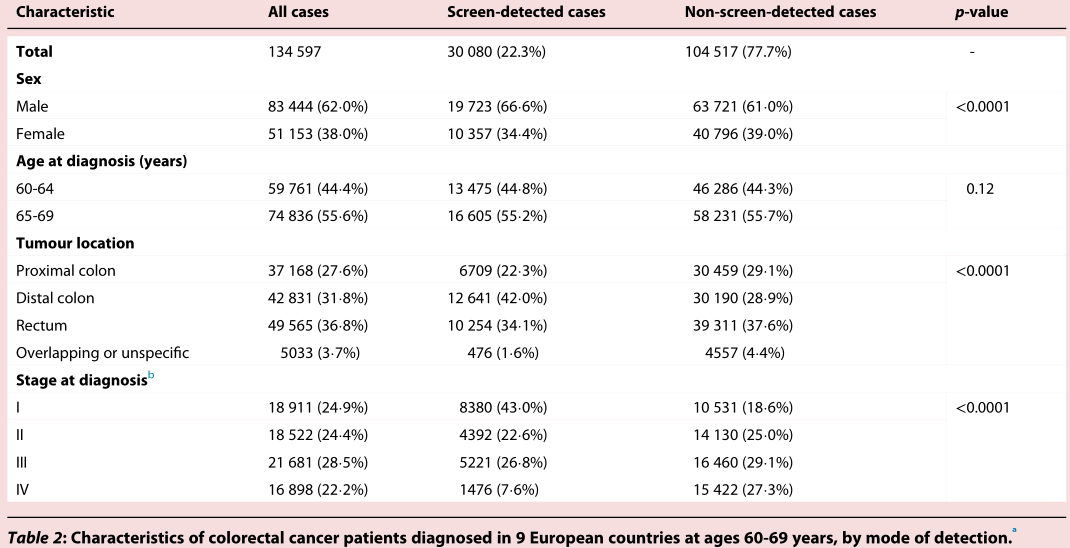
Figure 6 Crc patients with CRC patients with CRC patients with more early days and fewer late stages
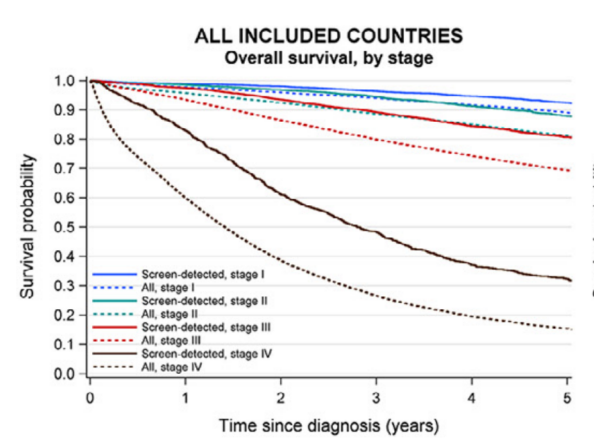
Figure 7 Each staged screening detection and testing CRC patients are better than the overall CRC patient
Regardless of the method of screening and testing, the total survival period of the detected CRC patients is much higher than the sum of the cancer patients and all patients that have not been detected. (Figure 8)
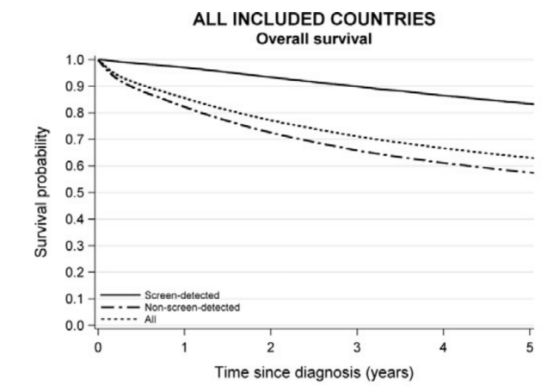
Figure 8 Screening detects the comparison of CRC and non -screening to detect CRC's five -year survival rate
Although this study has various bias, it is not to prove that screening can effectively reduce CRC burden.
However, it can be seen from the data that the prognosis of CRC is better than the prognosis of CRC diagnosed by screening.
At present, CRC is on the rise in young adults (<50 years old) and has a good prognosis of CRC. The general population should be encouraged to do CRC screening.
How to conduct scientific and reasonable early colorectal screening? The author combined with the "Chinese Circle Cancer Screening and Early Premature Creation Guide (2020, Beijing)" [8] to introduce the readers in detail the prefabricated symptoms, screening tools, screening strategies, risk factors, and protection factors.
▌ Pre -drive symptoms
The symptoms of colorectal cancer include abdominal pain, black stool (bleeding of digestive tract), abdominal mass, weight loss, and changes in bowel habits. About 40%of CRC patients have no obvious symptoms, so the guide recommends that the general population is 40-75 years old and receives the risk assessment of colorectal cancer.
(Recommended evaluation as low -risk people undergoing colorectal cancer screening at the age of 50 to 75; people with high risk of high -risk are screened from the age of 40 to 75; and if there are one or above one or above Class relatives suffer from colorectal cancer. It is recommended that the starting age of colorectal cancer screening is 40 years old or the youngest patients in the first -level relatives are 10 years in advance.)
▌ Screening tool
Colonoscopy and immune manure hidden blood test (FIT) are the two tools recommended by the guide.
Colonoscopy: In the current research and clinical practice, colonoscopy is a gold standard for colorectal cancer screening. Endoscopy can fully check the entire colorectal under the visual lens. You can take the tissue biopsy to further clarify the pathological diagnosis. It is currently recommended to perform high -quality colonoscopy every 5 to 10 years.
FIT: The most important means for colorectal cancer non -invasive screening. The main technical principle of FIT is to detect human hemoglobin in the fecal specimen through specific antibodies, and then indicate possible intestinal lesions. It is currently recommended to perform FIT detection once a year.
Figure 9 "Guide" strongly recommends colonoscopy and FIT

: Screening strategy: one scoring and two question volumes + initial screening experiments
Like most international countries, my country implements two -step screening strategies, combined with high -risk population identification (using questionnaire -based risk assessment and immune feces hidden blood test) and subsequent colonoscopy; the regular follow -up strategy of the general population.
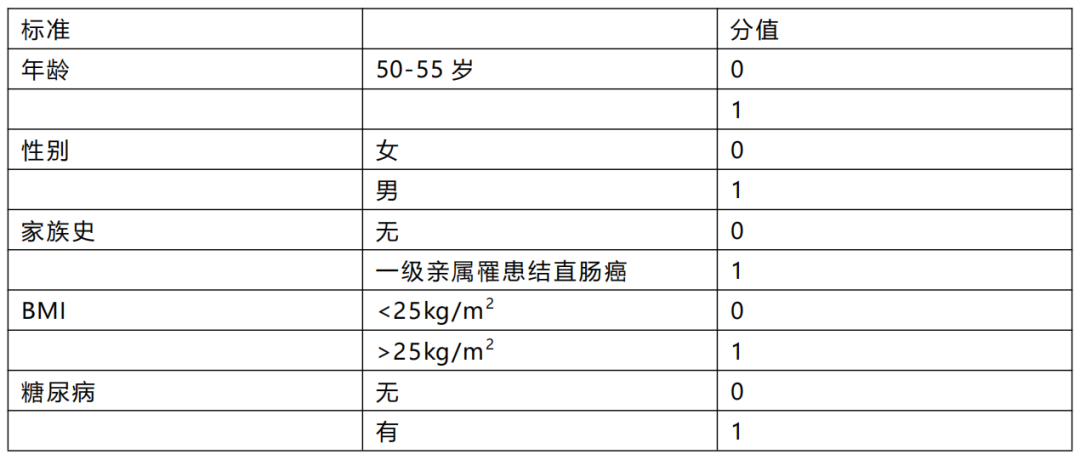
Announcement of colorectal screening score: Based on the age, gender, smoking, colorectal cancer family history, weight index (BMI) and self -prosecution diabetes systems based on the symptoms of Chinese non -symptoms The overall risk of rectal cancer is 0 ~ 2 points is low risk, and 3 to 6 points are high risk.
Table 1 Symptoms of non -symptoms colon screen screening scoring table
Community screening questionnaire: strong universality, wide community screening and self -inspection
Those who meet any of the following one or more are listed as high -risk people
First, first -level relatives have a history of colorectal cancer
2. I have a history of cancer (any history of malignant tumor disease)
3. I have a history of intestinal polyps
Fourth, at the same time, two or more people
1. Chronic constipation (the constipation in the past two years is more than 2 months)
2. Chronic diarrhea (the cumulative diarrhea in the past two years has continued for more than 3 months, and the time of each attack lasts more than 1 week)
3. Smooth blood
4. The history of bad life incidents (occurred in the past 20 years, and caused greater mental trauma or pain after the occurrence)
5. History of chronic appendicitis or appendix cutting
6. History of chronic biliary disease or history of gallbladder resection
Hospital screening questionnaire: generally guided by doctors professional
One of the following 6 cases can be used as high -risk people
1. Symptoms of digestive tract, such as blood, mucus, and abdominal pain: unknown cause anemia or weight loss
Second, there is a history of colorectal cancer
Third, there is a history of colorectal cancer (rectal tumor, ulcerative colitis, Crohn disease, hemorphosis, etc.)
Fourth, a direct relative with a family history of colorectal cancer
Fifth, there is a direct relative of the history of the intestinal polyps family
6. History of pelvic radiotherapy
How much is the risk factors?
The cause of colorectal cancer is not clear, but a large number of research evidence indicates that the occurrence of colorectal cancer is the result of the common effects of genetic, environmental and lifestyle.
The family history of colorectal cancer is a risk factor for colorectal cancer
The family history of colorectal cancer is related to the increased risk of colorectal cancer. A queue study in my country shows that the risk of women with colorectal cancer in first -level relatives is 2.07 times that of the risk of ordinary people.
Inflammatory bowel disease is a risk factor for colorectal cancer
A Meta analysis carried out by Jess was incorporated into 8 studies. The results showed that the risk of colorectal cancer in patients with ulcerative colitis was 2.4 times that of ordinary people.
Red meat and processing meat intake are the risk factor of colorectal cancer
Each daily intake of processed meat increases by 50g, and the risk of colorectal cancer incidence increases by 16%;
Each daily intake of red meat increases by 100g, and the risk of colorectal cancer incidence increases by 12%.
Diabetes is a risk factor for colorectal cancer
The risk of colon cancer and rectal cancer in patients with diabetes is 1.38 times and 1.20 times of healthy people, respectively.
Obesity is a risk factor for colorectal cancer
Each of the physical index increases 5kg/m2, the risk of colorectal cancer incidence increases by 5%; for each increase of 10 cm of the waist circumference, the risk of colorectal cancer incidence increases by 2%.
Smoking and drinking a lot of alcohol is a risk factor for colorectal cancer
What methods can reduce risks?
Taking aspirin is a protective factor for colorectal cancer
A forward -looking study in my country shows that the risk of colorectal cancer of Aspi is reduced.
However, there are currently reports that the prevention effect of colorectal cancer is limited. In 2022, the US prevention service team withdrew the recommendation of aspirin's prevention effect on colorectal cancer. Considering that aspirin taking the risk of complications such as gastrointestinal bleeding, the application of aspirin still needs to be carried out under the guidance of professional physicians.
The intake of dietary fiber, whole grain, and dairy products is the protection of colorectal cancer
The WCRF/AICR 2018 Report on "Diet, Nutrition, Body Activity and Cancer Prevention" reports:
Each daily dietary fiber intake increases by 10g, the risk of colorectal cancer is reduced by 9%;
Each daily intake of whole grains increases by 30g, and the risk of colorectal cancer is reduced by 5%;
Each daily intake of dairy products increases by 400g, and the risk of colorectal cancer is reduced by 13%.
Reasonable physical exercise is the protection of colorectal cancer
A queue study incorporated into 6,1321 Chinese in Singapore found that compared with people who do not conduct high -intensity and physical activity, a high -intensity physical activity of not less than half an hour can reduce the incidence of colorectal cancer by 15%.
references:
[1].Sung H,Ferlay J,Siegel RL,Laversanne M,Soerjomataram I,Jemal A,Bray F.Global Cancer Statistics 2020:GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries.CA Cancer J Clin.2021 May; 71 (3): 209-249.doi: 10.3322/CAAC.21660.epub 2021 Feb 4.pmid: 33538338.https: //pubmed.ncbi.nlm.gov/33538338/
[2].C.A.Doubeni,J.M.Major,A.O.Laiyemo,et al.,Contribution of behavioral risk factors and obesity to socioeconomic differences in colorectal cancer incidence,J.Natl.Cancer Inst.104(18)(2012)1353–1362. http://refhub.elsevier.com/s0304-3835 (21)00495-x/sref2
[3] .j.zhou, R.Zheng, S.Zhang, et al., Colorectal Cancer Burden and Trends: Comparison Between CHINA and Major Burden Countrld, chin.j.canc.res.33 (1) (1) (1) (1) (1) (1) (1) (1) (1) (1) (1) (1) (1) (1) (1) (1) (1) (1) 2021) 1 - 10.https://pubmed.ncbi.nlm.nih.gov/33707923/
[4] .zeng h, Chen W, Zheng R, ZHANG S, JI JS, ZOU X, XIA C, Sun K, Yang Z, Li H, WANG N, Han R, Li H, Mu h, he, he, he, he, he, he, he, he, he, he Y, xu y, fu z, zhou y, jiang j, yang y, chen j, wei k, fan d, wang j, fu f, zhao d, song j, jiang c, zhou x, gu, Jin F, Li Q, Li Y, Wu T, YAN C, DONG J, HUA Z, BAADE P, BRAY F, JEMAL A, Yu XQ, He J.Changing Cancer Survival in China During 2003-15: a Pooled Analysis of 17 Popuration-BASED Cancer Registries.lancet Glob Health.2018 May; 6 (5): E555-E567.Doi: 10.1016/S2214-109x (18) 30127-x.pmid: 29653628.https: //pubmed.ncbang.ncbang.ncbang.ncbang.ncbang.ncbang.ncbang.ncb. .nih.gov/29653628/
[5].Holleczek B,Rossi S,Domenic A,Innos K,Minicozzi P,Francisci S,Hackl M,Eisemann N,Brenner H;EUROCARE-5 Working Group:.On-going improvement and persistent differences in the survival for patients With colon and RECTUM CANCER ACROSS EUROPE 1999-2007-Results from the Eurocare-5 Study.eur J Cancer.2015 Oct; 51 (15): 2158-2168.doi: 10.1016/J.EJCA.2015.07.024.epub 26.pmid: 26421819.https: //pubmed.ncbi.nlm.nih.gov/26421819/ [6] .R.l.siegel, k.d.miller, a.goding sauer, et al., COLORECTAL CANCER Statistics, 2020, CACACA, CANC .J.clin.70 (3) (2020) 145–164.https: //acsjournals.onlinelibrary.com/doi/full/10.332/caac.21601
[7] .Cardoso R, Guo F, Heisser T, de Schutter H, Van Damme N, Nilbert Mc, Christensen J, Bouvier AM, Bouvier V, Launoy G, Worldoff AS, Cariou M, Robaszkiewicz M , WALSH PM, Senore C, Rosso S, Lemmens Vepp, Elferink magnet H.Overall and stage-specific survival of patients with screen-detected colorectal cancer in European countries:A population-based study in 9 countries.Lancet Reg Health Eur.2022 Jul 6;21:100458.doi:10.1016/j.lanepe. 2022.100458.pmid: 35832063; PMCID: pmc9272368.https: //pubmed.ncbi.nlm.nih.gov/35832063/
[8]. Guide to screen for screening and early early treatment of colon cancer (2020, Beijing) .https: ///kns.cNki.NT/kms/detable.aspx? Dbcode = cjfddtbname = zHzLTLATFORM -vkxvnz1g5_YB_VGIT8DLKLTEREMNJYSJIJVNDB7jdzoe3chx40y2jnxu
The first release of this article: the medical world tumor channel
Author of this article: Akai
Editor in charge: Sweet
- END -
Anime interpretation "1+20" policy ⑰

JPEG Webkit-Playsinline (The effect of horizontal screen viewing is better)Hebei...
As soon as I fall in love, I will blow up, and this show is revitalized by her
The summer vacation is here, and the life of adults is even harder.Not only can I ...