What is the occurrence of NSCLC, which is common and rare target mutations?What new progress?
Author:Cancer Channel of the Medical Time:2022.07.10
*For medical professionals for reading reference

One article clarified!
The incidence of brain metastases of patients with positive NSCLC patients with mutation is higher. The rapid development of molecular targeting drugs provides more treatment methods for patients with NSCLC brain metastases, which to a certain extent improves the survival and quality of life of NSCLC brain metastases. This article summarizes the relevant data of the intracranial relief of NSCLC brain metastasis in recent years to readers.
Nine recognized driving genes in the field of non -small cell lung cancer
For the IPASS study of the Asian population [1], the prelude to the targeted therapy of lung cancer, and also opened the new epidermal growth factor receptor (EGFR) mutant positive non -small cell lung cancer (NSCLC) tyrosine kinase inhibitor TKI individualized therapy era. With the development of genetic testing technology, more and more NSCLCs have been proven to have mutations in driving genes. The genetic gene drove normal cells into cancer cells, enabling cancer cells to survive, replicate, diffuse, and evolve for a long time. These genetic mutations are also called driver mutations, and they are also called "targets". Some molecular targeted drugs are designed specifically for them.
Figure 1 lists the type of drive gene mutation and frequency of NSCLC [2]. At present, there are nine recognized drive genes in the NSCLC field, including EGFR, KRAS, ALK, MET, ROS1, HER2, Braf, RET and NTRK. In China, there are many patients who drive mutations positive. There are research [3] showing about 73.9%of Chinese NSCLC patients with at least one national comprehensive cancer network (NCCN) guide related variation, of which the proportion of EGFR genome changes (including mutations and amplification) and ALK gene fusion are respectively. 50.1%and 7.8%, significantly higher than Western population.
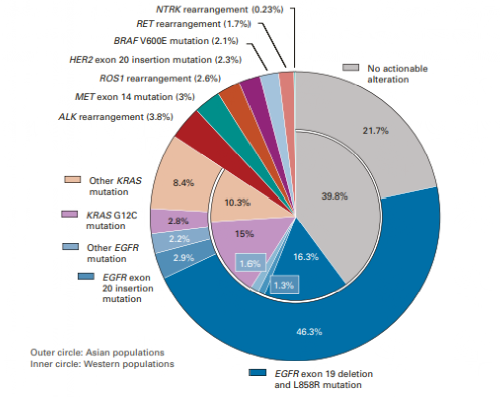
Figure 1: The incidence of mutation of targeted driving genes in lung adenocarcinoma
The incidence of brain metastases of patients with a positive NSCLC patients with a higher brain metastlashes is higher
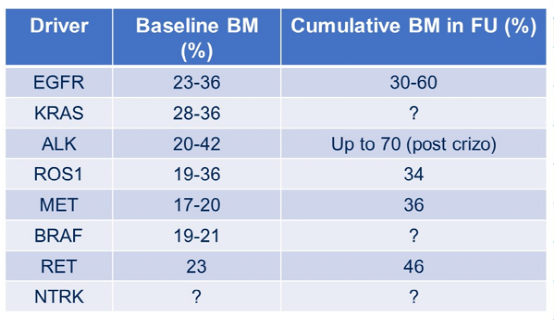
With the continuous exploration of targeted therapy and the successful research and development of related targeting drugs, more patients will benefit from targeted precision treatment. However, once NSCLC patients have brain metastases, the prognosis is still poor. About 20%-40%of NSCLC patients will have brain metastases [4]. Among NSCLC patients with carcinogenic drive mutations such as EGFR, ALK, ROS1, Braf, and KRAS, the incidence of brain metastases is higher, the baseline is 30%-40%[5], the cumulative incidence of disease is as high as 60%-70%[ 6].
Table 1: The incidence of baseline and cumulative brain metastases [6]
NSCLC brain metastases include local (surgery and radiotherapy) and systemic treatment (molecular targeted drugs, chemotherapy and immunotherapy). Doctors need to consider many factors in clinical decisions. Before starting treatment, whether there are symptoms to evaluate whether the early local treatment is required, controlling toxic risk, and the needs of external skull diseases. At the same time, it is necessary to evaluate what patients can benefit from whole body treatment. Clinicians need to understand the intracranial and extraterioxis relief rates of various treatment methods, the start time of the treatment reaction, the risk of pseudo -progress after immune treatment, and delayed delayed Toxic risk of radiotherapy. The ultimate goal of treatment is to treat metastatic lesions, improve patients' symptoms and quality of life, and extend the time of the patient's survival to the greatest extent.
A targeted therapy extends the survival of patients with brain metastases and improves the quality of life
In the past, the treatment methods of NSCLC brain metastasis are mostly limited to radiotherapy and chemotherapy. According to special diagnosis and evaluation of the prognosis grading system (DS-GPA), only patients with a score of more than 3.5 obtain a median total survival (OS); 7]; 7];; 7]; A phase III clinical study compared with early radiotherapy and delayed whole brain radiotherapy showed that there was no difference in efficacy between the two and the median OS was lower than half a year [8].
In recent years, the rapid development of molecular targeted therapy has provided more treatment methods for patients with NSCLC brain metastases, which has improved the survival and quality of life of NSCLC brain metastases to a certain extent.
1. EGFR
Flaura's analysis results show that for patients with EGFR mutations positive with brain metastases, Oshitinib significantly extended the progress of the disease to 15.2 months, a 53%risk of intracranial diseases from the first generation of EGFR-TKI [9].
2. ALK
CROWN's analysis of the Asian group shows that for ALK -positive NSCLC patients, the Ollantinib group's intracranial objective relief rate (ORR) is as high as 83.3%, of which 72.2%of the baseline is accompanied by patients with measuring brain metastatic lesions to use Lolatininib to use Lolatininib to use Lolatininib. Reaching the intracranial relief (CR), reflecting the amazing brain ability of Lolatinib [10].
3. Met14 outer show jump jump mutation mutation
在中国获批的首个MET-TKI赛沃替尼的Ⅱ期研究事后分析显示,患者的颅内病灶均在赛沃替尼治疗后有所缩小或保持稳定,其中有3例达到部分缓解( PR), 15 patients' skull lesions Orr reached 46.7%, and the median OS of patients with brain metastases reached 17.7 months. It is prompted to obtain significantly from the NSCLC brain metastases of Met14 outer appearance. Benefit [11,12].
In addition, in the clinical II study of Capmatinib and TEPOTINIB, 13 and 15 patients with brain metastases and intracranial efficacy were included in 13 cases and 15 cases. CAPMATINIB controlled the intracranial lesions of 12 patients, 7 of which reached intracranial relief, including 4 cases of complete relief (CR) [13]; 13 of the 15 patients treated with TEPOTINIB were controlled Including 3 CR, 9 PR and 1 case of stable disease (SD) [14]. The above data suggests that these two MET-TKIs are used in intracranial lesions. 4.kras G12C
Targeted therapy has greatly improved the survival time of patients, and adverse reactions are controllable. The new generation of targeted drugs has achieved encouraging results in controlling brain metastases. At the 2022 ASCO Annual Meeting, a major research results of NSCLC brain metastatic targeting therapy were released. Krystal-1 studies discovered for the first time that ADAGRASIB showed activity in the active central nervous system (CNS) to KRAS G12C mutation NSCLC [15].
In the Study-I/II-II phase I/II phase IB phase study research, Adagrasib obtained 32%ORR with KRAS G12C mutations, unbustored active central nervous system metastasis, and 84%of 84% Disease control rate. In addition, during the assessment of lumbar spine puncture, Adagrasib shows an excellent CNS concentration, which is 0.47 in the average concentration ratio (KP, UU) of the intensive effusion and plasma, which is higher than the other known intracranial active drugs observed in the intracranial active drugs. Concentration ratio. As we all know, KRAS is a difficult target. In the future, more R & D data will break through expectations.
NSCLC brain metastasis targeted therapy and future prospects
The extensive use of targeted drugs to a certain extent change the treatment strategy of driving the genetically -positive NSCLC brain metastasis. The precision medicine era needs to be based on multidisciplinary teams. Whether there are symptoms in the brain metastases, the status of the skull disease, and the characteristics of NSCLC molecular genome and PD-L1 expression) determine the treatment strategy [16,17]. But one of its main limitations is that patients with NSCLC and unprepared brain metastases are usually excluded from random clinical studies evaluating systemic treatment. With the increasing incidence of patients with brain metastases, and the emergence of clinical research in patients with integrated or specifically targeting patients with brain metastases, this situation is changing.
What is the future NSCLC of the driving mutant gene, Professor Lizza Hendriks put forward the point of view at the 2022 ASCO annual meeting: ① Use liquid biopsy technology such as cerebral spine (CSF) to track the drug resistance mechanism of EGFR-TKI in CNS; ② Follow the current evaluation TKI TKI Dose increasing research (NCT04739358); ③ The data of Ostenib single medicine may not be ideal, chemotherapy combined with anti -vascular production drugs may improve the clinical ending of patients to patients (NCT02971501, NCT02521051); The incidence of brain metastases is correlated, and the systemic treatment plan is adjusted according to the common mutation; ⑤ "Do you continue to continue the TKI treatment when the whole body progresses to control the CNS? Can CNS progress while the TKI treatment can be performed at the same time?" It is still a controversial topic. It is necessary to further work to guide clinical decisions in different reactions.
references:
[1] MOK TS, ETAL. Gefitinib or Carboplatin-Paclitaxel in Pulmonary Adenocarcinoma. N English J Med. 2009 SEP 3; 361 (10): 947-57.
[2] TAN AC, TAN DSW. Targeted therapies for LUNG CANCER PATIENTS With Oncogenic Driver Molecular Alterations.
[3] Wen S, ETAL. Genomic Signature of Driver Genes Identify by Target Next-Generation Sequencing in Chinese Non-Small Cell LUNG CANCER. Oncologist.
[4] Villano JL, et al. Incident of Brain Metastasis at initial presentation of Lung Cancer. Neuro oncol. 2015 Jan; 17 (1): 122-8. [5] Patil T, et al. Incide of bra Stage Iv Ros1-Rearranged Non-Small Cell Lung Cancer and Rate of Central Nervous System Progression on Crizotinib.
[6]Schoenmaekers JJAO, et al. Central nervous system metastases and oligoprogression during treatment with tyrosine kinase inhibitors in oncogene-addicted non-small cell lung cancer: how to treat and when? Transl Lung Cancer Res. 2020 Dec;9(6) : 2599-2617.
[7]Sperduto PW, et al. Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: a multi-institutional analysis of 4,259 patients. Int J Radiat Oncol Biol Phys. 2010 Jul 1;77( 3): 655-61.
[8]8Robinet G, et al. Results of a phase III study of early versus delayed whole brain radiotherapy with concurrent cisplatin and vinorelbine combination in inoperable brain metastasis of non-small-cell lung cancer: Groupe Français de Pneumo-Cancérologie (GFPC) Protocol 95-1. Ann oncol. 2001 Jan; 12 (1): 59-67.
[9] Ramalingam SS, et al; Flaura Investigators. Overall Survival with Osimrtinib in Untreated, EGFR-MUTATED Advanced NSCLC. N ENGL J Med. 2020 Jan 2; 382 (1): 41-50.
[10]Benjamin J. Solomon, et al. Updated Efficacy and Safety From the Phase 3 CROWN Study of First-Line Lorlatinib vs Crizotinib in Advanced Anaplastic Lymphoma Kinase (ALK)–Positive Non-Small Cell Lung Cancer (NSCLC). AACR2022, Abstract #ct223.
[11]Lu S, et al. Once-daily savolitinib in Chinese patients with pulmonary sarcomatoid carcinomas and other non-small-cell lung cancers harbouring MET exon 14 skipping alterations:a multicentre, single-arm, open-label, phase 2 study [J].The Lancet Respiratory Medicine,2021,9(10):1154-1164.[12]Lu S, et al.2MO Final OS results and subgroup analysis of savolitinib in patients with MET exon 14 skipping mutations(METex14+)NSCLC [J]. Annals of oncology, 2022, 33 (s2): s27.
[13] Wolf J, SETO T, Han J Y, Et Al. Capmatinib in Met Exon 14 – Mutated or Met-Amplify Non-Cell LUNG CANCER [J]. New England Journal of Medicine, 2020, 383 (10): 944-957.
[14]Le X, Sakai H, Felip E, et al. Tepotinib Efficacy and Safety in Patients with MET Exon 14 Skipping NSCLC: Outcomes in Patient Subgroups from the VISION Study with Relevance for Clinical Practice[J]. Clinical Cancer Research, 2022 , 28 (6): 1117-1126.
[15] OU SI, ET Al. FIRST-In-Human Phase I/IB Dose-Finding Study of Adagrasib (MRTX849) in Patients with Advanced Krasg12c Solid Tumors (Krystal-).
[16] Vogelbaum ma, et al. Treatment for brain metastases: asco-sno-candro guideline. J clin oncol. 2022; 40: 492-516.
[17]Le Rhun E, et al; EANO Executive Board and ESMO Guidelines Committee. EANO-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up of patients with brain metastasis from solid tumours. Ann Oncol. 2021;32:1332- 1347.
*This article is only used to provide scientific information to medical people, and does not represent the viewpoint of this platform


- END -
AI open prescription?Is 250,000 doctors reliable online?

Which doctor is right?Earlier this year, Xia Liang, who lives in Changde, Hunan, w...
New discoveries | intestinal flora can affect obesity!

Obesity is a global public health issue. Some research predicts that in 2030, the ...